The prevalence of obesity in the United States has become a pressing public health concern, with significant variations across different states and demographics.
Recent data from 2021-2023 indicates that over 40% of American adults have obesity, with certain states and regions experiencing even higher prevalence.
The Midwest and South have been particularly affected, with obesity prevalence reaching as high as 36.0% and 34.7%, respectively.
Key Takeaways
- Obesity prevalence varies significantly across different states and regions in the United States.
- The Midwest and South have the highest prevalence of obesity.
- Certain demographics, such as non-Hispanic Black adults, have a higher obesity prevalence.
- Education level and age are significant factors in obesity prevalence.
- Public health implications of rising obesity rates are substantial, with significant economic impacts on healthcare systems.
The Current State of Obesity in America
Understanding the current state of obesity in America requires a closer look at the statistics and definitions surrounding this condition. Obesity is a complex health issue that affects a significant portion of the population.
Defining Obesity and BMI Classifications
Obesity is typically defined using the Body Mass Index (BMI) measurement system. BMI is calculated as weight in kilograms divided by height in meters squared. For adults, BMI classifications are as follows: a BMI of 18.5 to 24.9 is considered normal or healthy weight, 25 to 29.9 is overweight, 30 or above indicates obesity, and 40 or above is classified as severe obesity.
The use of BMI as a screening tool allows healthcare professionals to identify potential weight-related health risks at the population level. Although BMI has its limitations, it remains a widely accepted metric for assessing obesity.
Fast Facts on US Obesity Prevalence
According to recent data from 2021-2023, the prevalence of obesity among adults in the United States was 40.3%. The prevalence was 39.2% in men and 41.3% in women, indicating a slight difference between genders. These statistics highlight that over 40% of US adults currently have obesity.
- The prevalence of obesity varies slightly between men and women, with women having a higher rate.
- Obesity is categorized into different classes based on BMI, with 30+ indicating obesity and 40+ indicating severe obesity.
- The data suggests that obesity is a significant public health issue across the US population.
These fast facts underscore the importance of addressing obesity as a public health concern. Understanding the definitions and prevalence rates is crucial for developing effective interventions.
Understanding US Obesity Rates
The prevalence of obesity in the United States is a growing concern that requires a comprehensive understanding of its current rates. Obesity is a significant public health issue, affecting millions of Americans and contributing to various health complications. To effectively address this epidemic, it’s essential to examine the latest data on obesity prevalence and how it varies across different demographics.
National Prevalence Data 2021-2023
The National Health and Nutrition Examination Survey (NHANES) is the primary source for obesity data in the United States. According to the NHANES data from 2021 to 2023, the age-adjusted prevalence of obesity in adults did not change significantly compared to the period from 2013-2014. However, the age-adjusted prevalence of severe obesity increased from 7.7% to 9.7% during the same period. This indicates a concerning trend where severe obesity is becoming more prevalent, even if overall obesity rates appear stable.

The data from NHANES provides a comprehensive picture of obesity prevalence in the US. It highlights the need for continued public health efforts to address the growing issue of severe obesity.
Demographic Breakdown by Age and Sex
Analyzing obesity prevalence by age and sex reveals significant variations. The prevalence of obesity in adults aged 40-59 was 46.4%, higher than in adults aged 20-39 (35.5%) and those 60 and older (38.9%). This pattern was consistent in both men and women, indicating that middle-aged adults are more likely to experience obesity. Understanding these demographic differences is crucial for tailoring public health interventions to effectively target high-risk populations.
The demographic breakdown also underscores the importance of considering age and sex when developing strategies to combat obesity. By examining these factors, healthcare professionals and policymakers can create more targeted and effective interventions to reduce obesity rates across different demographic groups.
Obesity Trends Across Different Demographics
The US obesity epidemic has distinct trends across different racial, ethnic, and socioeconomic groups. Understanding these trends is crucial for developing targeted interventions to address the obesity crisis.
Racial and Ethnic Disparities
Obesity prevalence varies significantly across different racial and ethnic groups. Nearly 1 in 2 non-Hispanic Black adults (49.6%) have obesity, compared to more than 2 in 5 non-Hispanic white adults (42.2%) and nearly 1 in 2 Hispanic adults (44.8%). In contrast, more than 1 in 6 non-Hispanic Asian adults (17.4%) have obesity. These disparities suggest that genetic, cultural, and environmental factors contribute to the differences in obesity prevalence among these groups.
Socioeconomic Factors and Education Level Impact
The prevalence of obesity is also influenced by socioeconomic factors, including education level. Adults with a bachelor’s degree or more have a lower obesity prevalence (31.6%) compared to those with less education. The difference in obesity prevalence between adults with a high school diploma or less (44.6%) and those with some college (45.0%) is not significant. No significant differences in obesity prevalence by education level were observed between men and women. Socioeconomic factors such as income, occupation, neighborhood resources, and food security also play a crucial role in determining obesity risk across different demographic groups.
Analyzing these demographic trends over time can provide insights into the underlying social determinants of health that contribute to obesity disparities. By understanding these factors, policymakers and healthcare professionals can develop more effective strategies to address the obesity epidemic.
State-by-State Obesity Comparisons
A closer look at obesity data across the US states reveals stark contrasts in obesity prevalence, highlighting regional health disparities. The United States exhibits a complex landscape when it comes to obesity rates, with significant variations observed across different states.
Highest Obesity Rates
Some states stand out for having particularly high obesity rates. West Virginia leads the nation with an obesity prevalence of over 50% among males. Mississippi follows closely, with a significant obesity rate among females, reaching as high as 55.9%. Other states with notably high obesity prevalence include Louisiana and Alabama.
| State | Obesity Prevalence in Males (%) | Obesity Prevalence in Females (%) |
|---|---|---|
| West Virginia | 50.5 | 48.2 |
| Mississippi | 45.1 | 55.9 |
| Louisiana | 44.8 | 54.3 |
Regional factors contributing to these high rates may include socioeconomic status, access to healthy food options, and the prevalence of physical activity infrastructure.
Lowest Obesity Rates
On the other end of the spectrum, some states have managed to maintain lower obesity rates. Colorado, Hawaii, and Washington DC are notable for their lower obesity prevalence. Hawaii, for instance, has an obesity prevalence of 63.7% among women, one of the lowest in the country.
| State | Obesity Prevalence in Males (%) | Obesity Prevalence in Females (%) |
|---|---|---|
| Colorado | 38.2 | 36.5 |
| Hawaii | 35.1 | 33.7 |
| Washington DC | 34.5 | 32.9 |
These states often have policies and cultural factors in place that promote healthier lifestyles, such as access to green spaces, healthy food initiatives, and community programs encouraging physical activity.
Understanding these state-by-state differences is crucial for developing targeted interventions to combat the obesity epidemic across the United States.
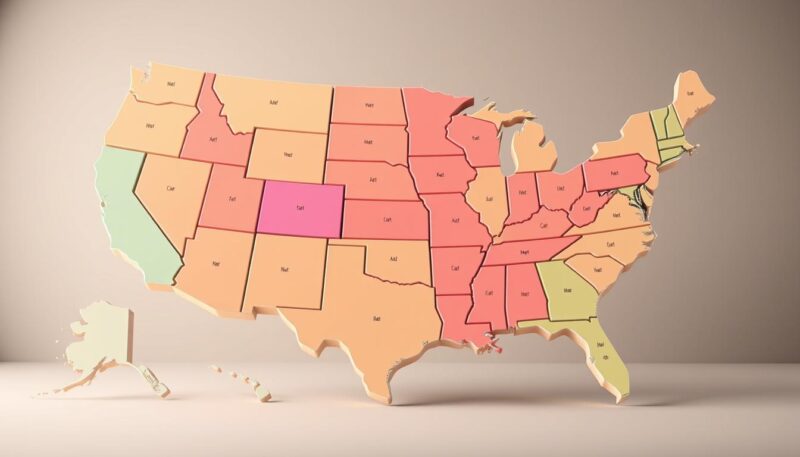
Regional Patterns in US Obesity Rates
Regional patterns in obesity rates across the US reveal critical insights into the nation’s health landscape. The prevalence of obesity varies significantly across different regions, influenced by a complex array of factors including socioeconomic conditions, food environments, and physical activity infrastructure.
The Midwest and Southern states have been identified as having particularly high obesity rates. The highest obesity-related death rates were seen in Midwestern states such as Illinois, Indiana, and Ohio. Southern states like Mississippi, Louisiana, and Alabama also report some of the nation’s highest obesity prevalence rates, particularly among women.
Midwest and Southern States Analysis
The Midwest and Southern United States are often referred to as the “obesity belt” due to their high obesity prevalence rates. Mississippi, for instance, has an obesity prevalence rate of 55.9% among adult females. Factors contributing to these high rates include limited access to healthy food options and inadequate physical activity infrastructure.
| Region | Obesity Prevalence Rate (%) | Obesity-Related Death Rate |
|---|---|---|
| Midwest | 35-40 | High |
| Southern | 40-45 | High |
| Northeastern | 25-30 | Low |
| Western | 20-25 | Low |
Northeastern and Western States Analysis
In contrast, Northeastern and Western states generally have lower obesity rates. States like Colorado and Hawaii report some of the lowest prevalence rates of overweight and obesity. These regions tend to have better access to healthy food options, more opportunities for physical activity, and different cultural dietary patterns.
Understanding these regional differences is crucial for developing targeted interventions to address the obesity epidemic. By examining the factors that contribute to lower obesity rates in certain regions, policymakers can develop more effective strategies to improve public health across the United States.
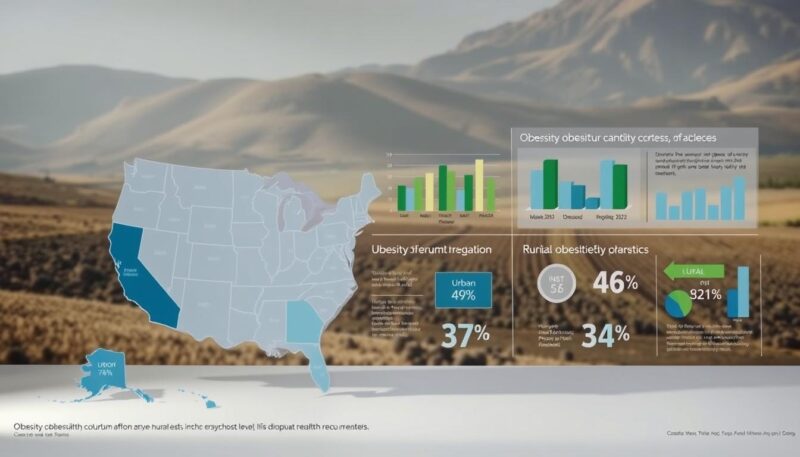
Urban vs. Rural Obesity Prevalence
The urban-rural divide in obesity prevalence is a pressing issue in American public health. Obesity rates are consistently higher in non-metropolitan areas compared to urban centers, highlighting a significant health disparity.
Differences Between Metropolitan and Non-Metropolitan Areas
Studies have shown that individuals living in rural areas have a higher risk of obesity-related mortality, with age-adjusted death rates of 4.0 per 100,000 people compared to 2.9 in urban areas according to recent research. This disparity is attributed to various factors, including limited access to healthcare services and fewer recreational facilities in rural settings.
Environmental Factors Contributing to Obesity
Environmental conditions play a crucial role in the higher obesity prevalence in rural areas. The lack of walkability, inadequate transportation infrastructure, and reduced availability of fresh foods contribute to an environment that promotes obesity. Furthermore, socioeconomic factors, including economic opportunities and educational resources, also impact health status and obesity risk.
Severe Obesity: A Growing Concern
Severe obesity, characterized by a BMI of 40 or more, poses substantial health risks and is increasingly prevalent among American adults. This condition affects approximately 9.4% of the adult population, representing a significant subset of those classified as obese.

Prevalence and Trends
The prevalence of severe obesity in adults was 9.4% during August 2021-August 2023. Notably, there has been an upward trend in severe obesity prevalence, increasing from 7.7% to 9.7% between 2013-2014 and 2021-2023. This rise is concerning, especially as overall obesity rates have remained relatively stable during the same period.
Significant disparities exist in the prevalence of severe obesity across different age groups and genders. Adults aged 40-59 have the highest prevalence at 12.0%, compared to 9.5% in those aged 20-39 and 6.6% in those aged 60 and older.
High-Risk Populations
The prevalence of severe obesity varies significantly between men and women. Women have a nearly twice higher prevalence rate (12.1%) compared to men (6.7%). Among men, the prevalence is highest in those aged 40-59, while among women, it is higher in those aged 20-39 and 40-59 compared to those aged 60 and older.
These high-risk populations are more likely to experience severe health complications, including type 2 diabetes, cardiovascular disease, mobility issues, and increased mortality rates. The implications for healthcare systems are substantial, highlighting the need for targeted interventions and support for those affected by severe obesity.
Childhood and Adolescent Obesity Statistics
The prevalence of obesity among children and adolescents in the United States has reached alarming levels, with significant implications for public health. Recent statistics indicate that more than one in five children aged 6-19 now have obesity, highlighting a critical issue that demands immediate attention.
Prevalence Among Different Age Groups
Obesity prevalence among youth varies significantly across different age groups. Among children aged 2 to 5, more than 1 in 8 (13.4%) have obesity. This rate increases to more than 1 in 5 (20.3%) among children and youth aged 6 to 11, and further to 21.2% among adolescents aged 12 to 19. These statistics underscore the need for targeted interventions across different age groups.
| Age Group | Obesity Prevalence |
|---|---|
| 2-5 years | 13.4% |
| 6-11 years | 20.3% |
| 12-19 years | 21.2% |
Projections for the Future
Projections indicate that by 2050, approximately 43 million American children and adolescents will have overweight or obesity, representing about one in three young people. This trend has significant long-term implications, including the potential for shorter lifespans, increased rates of early-onset type 2 diabetes, and substantial lifetime healthcare costs.

The data on childhood and adolescent obesity statistics paint a concerning picture of the current state of youth health in the United States. Understanding these trends is crucial for developing effective public health strategies to address this growing issue.
Historical Trends and Future Projections to 2025
Understanding the historical context of obesity rates is essential for predicting future trends and developing effective public health strategies. The United States has witnessed a significant shift in obesity prevalence over the past few decades.
Ten-Year Trend Analysis
From 2013-2014 through August 2021-August 2023, the age-adjusted prevalence of obesity in adults remained relatively stable, hovering around 40%. However, the age-adjusted prevalence of severe obesity increased from 7.7% to 9.7% during the same period. This indicates a concerning trend where overall obesity rates may have plateaued, but the more severe forms of obesity continue to rise.
| Year | Obesity Prevalence | Severe Obesity Prevalence |
|---|---|---|
| 2013-2014 | 40% | 7.7% |
| 2021-2023 | 40% | 9.7% |
The prevalence of obesity among children and adolescents aged 2 to 19 years roughly doubled between 1988-1994 and 2017-2018. This historical data is crucial for understanding the trajectory of obesity rates.
Statistical Modeling for 2025 Projections
Statistical modeling techniques are employed to generate projections for obesity rates in 2025, incorporating demographic shifts, economic factors, and public health interventions. According to forecasts, by 2050, approximately 213 million American adults and 43 million children and adolescents will have overweight or obesity.
“If current trends continue, the future burden of obesity-related health issues will be substantial, emphasizing the need for effective prevention and intervention strategies.”
Various scenarios for 2025 obesity rates are considered based on different assumptions about intervention effectiveness, policy changes, and societal trends. This analysis provides a range of possible outcomes rather than a single prediction, helping policymakers and public health officials prepare for different contingencies.

By examining historical trends and future projections, we can better understand the complex factors driving the obesity epidemic and develop targeted strategies to mitigate its impact.
Health Consequences of Rising Obesity Rates
The health consequences of rising obesity rates are far-reaching, impacting various aspects of an individual’s health and wellbeing. As obesity prevalence continues to grow, understanding its health implications becomes increasingly important.
Mortality Statistics Associated with Obesity
Between 1999 and 2020, the age-adjusted obesity-related death rate increased dramatically from 2.1 to 7.2 deaths per 100,000, marking an increase of more than 240%. This alarming rise underscores the need for comprehensive strategies to address obesity and its related health risks.
Obesity is associated with an increased risk of mortality due to various health conditions. The distribution of excess body fat, particularly visceral fat, plays a significant role in the risk of cardiovascular and metabolic diseases.
- Cardiovascular disease
- Type 2 diabetes
- Certain types of cancer
- Stroke
- Hypertension
Comorbidities and Associated Health Conditions
Obesity is linked to numerous serious health conditions beyond mortality. Excess body weight, particularly around the abdominal area, significantly increases the risk for various diseases, including type 2 diabetes, high blood pressure, heart disease, and certain cancers.
The metabolic consequences of obesity, such as insulin resistance, systemic inflammation, and hormonal disruptions, contribute to the development of these diseases. Furthermore, obesity affects multiple body systems, including respiratory function, musculoskeletal health, and psychological wellbeing.
Understanding these health consequences is crucial for developing effective interventions to reduce obesity rates and mitigate its impact on public health.
Economic Impact of the Obesity Epidemic
The obesity epidemic in the United States has significant economic implications that affect the nation’s healthcare system and overall economy. The direct healthcare costs related to obesity were estimated to be as high as $480 billion in 2016, a figure that continues to rise substantially.
Healthcare Costs Associated with Obesity
Obesity-related conditions such as heart disease, diabetes, and stroke drive healthcare spending through increased hospitalizations, medication use, and specialized care requirements. These conditions result in a significant economic burden on the healthcare system.
- Increased hospitalizations due to obesity-related complications
- Rise in medication use for managing obesity-related conditions
- Specialized care requirements for conditions like heart disease and diabetes
Productivity and Indirect Economic Effects
The indirect economic costs of obesity are also substantial, including reduced workforce productivity, increased absenteeism, disability payments, and premature mortality that removes skilled workers from the labor force. These factors contribute to the overall economic disadvantage faced by the United States due to the obesity epidemic.
As the prevalence of obesity continues to rise, it is essential to consider the future economic impacts, including the potential strain on Medicare, Medicaid, and private insurance systems.
Social Determinants of Health and Obesity
The social determinants of health play a crucial role in shaping obesity risk and contributing to disparities in obesity prevalence across different populations. Factors such as the environment in which people live, work, and play significantly influence their health behaviors and ultimately their body weight status.
One of the critical social determinants is access to healthy food options. Many low-income and minority neighborhoods function as “food deserts,” with limited access to affordable, nutritious food but an abundance of calorie-dense, nutrient-poor foods.
Access to Healthy Food Options
Communities with better access to healthy food options tend to have lower rates of obesity. Initiatives that improve food environments can help reduce obesity rates.
- Increasing the availability of healthy food retailers in underserved areas
- Supporting local food programs that promote healthy eating
- Improving food labeling to help consumers make informed choices
Physical Activity Infrastructure and Opportunities
Neighborhood safety, walkability, parks, recreational facilities, and transportation options also play a significant role in determining obesity risk. Communities that invest in physical activity infrastructure can encourage more active lifestyles.
As Dr. [Last Name] once said, “Creating environments that support physical activity is crucial for reducing obesity rates.”
Addressing these social determinants of health is essential for reducing obesity rates, particularly among disadvantaged populations facing structural barriers to healthy lifestyles.
Public Health Responses to Obesity Crisis
As obesity rates continue to rise, public health officials are responding with a range of interventions aimed at reducing obesity prevalence. The United States is grappling with an obesity epidemic that has significant implications for national health.
Federal and State Initiatives
The public health response to obesity involves various federal and state initiatives. The Healthy People 2030 goal, for instance, aims to reduce adult obesity prevalence to 36%. Currently, the prevalence stands at 40.3%, indicating a significant gap between the target and the current state. State-level policy approaches include implementing school nutrition standards, sugar-sweetened beverage taxes, menu labeling requirements, and physical education mandates. These initiatives are designed to promote healthier lifestyles and reduce obesity rates.
Effectiveness of Current Interventions
Despite numerous programs aimed at reducing obesity, the age-adjusted prevalence of obesity in adults has not decreased significantly in recent years. The American Heart Association’s new advisory focuses on addressing upstream social determinants of health, recognizing that tackling obesity requires more than just individual behavior change. Innovative public health approaches being tested include community-based participatory research, cross-sector collaborations, and health-in-all-policies frameworks. These approaches acknowledge that obesity is a complex systems problem requiring a multifaceted response.
The effectiveness of current interventions is mixed, with some showing promise while others have limited impact. Evaluating these interventions is crucial to understanding what works and what doesn’t in the fight against obesity. By focusing on the social determinants of health and implementing comprehensive strategies, public health officials hope to make a more significant impact on reducing obesity rates in the United States.
The Role of Medical Interventions
As obesity continues to affect a significant portion of the US population, the importance of effective medical treatments becomes increasingly evident. The growing obesity epidemic necessitates a multifaceted approach, including medical interventions that can help manage weight and mitigate related health issues.
Weight Management Medications and Treatments
Recent advancements in anti-obesity medications, such as GLP-1 receptor agonists, have shown unprecedented effectiveness in weight management. These medications work by regulating appetite and metabolism, potentially helping patients achieve a 15-20% body weight reduction, far exceeding the typical 5-10% achieved with lifestyle interventions alone. According to research published on the National Center for Biotechnology Information, such medications offer new hope for individuals struggling with obesity.
The introduction of these newer treatments has transformed the landscape of obesity care. However, their national impact could be limited by factors such as high costs, inequitable access, and variable long-term effectiveness.
Barriers to Accessing Obesity Care
Despite the availability of effective weight management medications, several barriers hinder access to obesity care. High medication costs, often exceeding $1,000 monthly, limited insurance coverage, provider shortages, and persistent weight stigma in healthcare settings all contribute to this issue.
| Barrier | Description | Impact |
|---|---|---|
| High Medication Costs | Costs often exceed $1,000 monthly | Limits accessibility for many patients |
| Limited Insurance Coverage | Inconsistent coverage across providers | Reduces treatment options for patients |
| Provider Shortages | Insufficient number of specialists | Delays treatment for those in need |
| Weight Stigma | Negative attitudes in healthcare settings | Discourages patients from seeking care |
Bariatric surgery is another critical treatment option for patients with severe obesity (BMI ≥40) or those with BMI ≥35 and obesity-related comorbidities. While it offers significant benefits, it also has limitations that need to be considered.
In conclusion, while medical treatments are crucial in addressing obesity, they cannot alone solve the epidemic. Concurrent public health approaches addressing underlying environmental and social factors are essential.
Prevention Strategies for Reducing Obesity Rates
Effective obesity prevention requires a combination of individual, community, and policy-level changes. Healthcare systems cannot manage the epidemic solely through lifelong secondary prevention policies. There is no vaccine for noncommunicable diseases like obesity. Yet, similar to infectious diseases, obesity is preventable in most cases, and its early signs are recognizable.
Addressing the obesity epidemic will therefore require both systemic interventions and a supportive cultural framework that encourages healthy lifestyles. This involves examining evidence-based prevention strategies that show promise for reducing obesity rates at the population level, emphasizing that prevention is more cost-effective than treatment.
Community-Based Approaches
Successful community-based approaches modify food and physical activity environments. Examples include farm-to-school programs, complete streets initiatives, workplace wellness programs, and faith-based health promotion. These programs have been shown to positively impact obesity risk factors by promoting healthier choices and increasing opportunities for physical activity.
| Program | Description | Impact |
|---|---|---|
| Farm-to-School | Integrates local produce into school meals | Increases fruit and vegetable consumption among children |
| Complete Streets | Designs streets to accommodate all users, including pedestrians and cyclists | Promotes physical activity and reduces traffic congestion |
| Workplace Wellness | Offers health promotion programs and healthy food options at work | Encourages healthy behaviors among employees |
According to a study published on the National Center for Biotechnology Information website, community-based interventions can be effective in reducing obesity rates.
Policy Recommendations
Leading health organizations recommend several policy changes to impact obesity risk factors. These include implementing sugar-sweetened beverage taxes, improving nutrition assistance programs, and enforcing physical education requirements. Such policies can help create an environment that supports healthy lifestyles and reduces the risk of obesity.
Early intervention in childhood is crucial for establishing healthy weight trajectories. Obesity prevention is more effective when started early, as reversing established obesity can be challenging. Effective prevention requires coordinated multi-level approaches that address individual behaviors, community environments, healthcare practices, and broader social and economic policies that influence body weight.
Conclusion: Addressing the US Obesity Epidemic
The escalating obesity rates in the United States represent a complex public health challenge that necessitates a comprehensive and coordinated response across various sectors. With 40.3% of American adults having obesity, the prevalence data underscores the urgency of the situation.
Significant disparities in obesity prevalence across different states, demographic groups, and socioeconomic strata highlight the need for targeted approaches. For instance, certain racial and ethnic groups, as well as populations with lower socioeconomic status, are disproportionately affected.
Addressing obesity requires a balanced strategy that combines evidence-based prevention, accessible treatment options, and policies that promote healthy choices. This includes improving access to healthy food options, enhancing physical activity infrastructure, and implementing effective public health interventions.
The current trends indicate a concerning trajectory, with projections suggesting continued increases through 2025 and beyond if left unchecked. Reversing these trends will necessitate sustained investment, innovative approaches, and collaboration across government, healthcare, business, education, and community sectors.
By synthesizing the key findings and data presented, it becomes clear that tackling obesity as a national priority is not only a health imperative but also an economic necessity. The health consequences of rising obesity rates, including increased mortality and comorbidities, alongside the substantial healthcare costs and indirect economic effects, underscore the urgency for collective action.
In conclusion, the United States must renew its commitment to addressing the obesity epidemic through a multi-faceted approach that is grounded in data-driven strategies and supported by collaborative efforts across different sectors.
FAQ
What is body mass index (BMI), and how is it used to define obesity?
Body mass index (BMI) is a measurement used to assess body weight relative to height. It is calculated by dividing a person’s weight in kilograms by the square of their height in meters. Obesity is typically defined as a BMI of 30 or higher.
What are the current obesity prevalence statistics among adults in the United States?
According to recent data from the National Health and Nutrition Examination Survey, more than two-fifths of adults in the United States have obesity, with significant variations across different age groups and demographics.
How do obesity rates vary across different racial and ethnic groups?
Obesity prevalence differs significantly among various racial and ethnic groups, with higher rates often observed among certain minority populations, highlighting the need for targeted interventions.
What are the most significant health consequences associated with obesity?
Obesity is linked to an increased risk of numerous health conditions, including heart disease, type 2 diabetes, certain types of cancer, and mental health disorders, underscoring the importance of addressing this public health issue.
What role do socioeconomic factors play in obesity prevalence?
Socioeconomic factors, including education level, income, and access to healthy food and physical activity opportunities, can significantly influence obesity risk, with disadvantaged populations often facing greater challenges.
What public health initiatives are being implemented to combat the obesity epidemic?
Various federal and state initiatives are underway to address obesity, including efforts to improve nutrition education, increase access to healthy food and physical activity opportunities, and promote evidence-based interventions.
How can community-based approaches contribute to reducing obesity rates?
Community-based initiatives, such as promoting healthy eating habits, enhancing physical activity infrastructure, and supporting local food systems, can play a crucial role in preventing obesity and promoting overall well-being.
What is severe obesity, and how is it defined?
Severe obesity, also known as class II or III obesity, is typically defined as a BMI of 35 or higher, and is associated with a significantly increased risk of serious health complications and mortality.
What are the projected obesity trends for the next generation?
Based on current data and statistical modeling, obesity prevalence is expected to continue rising, with potentially severe consequences for public health and the economy unless effective interventions are implemented.
